Yes, breast reduction is a covered service by health insurance if certain criteria are met. What those criteria are depends on the insurance and the state. All companies require that the large breasts cause significant symptoms and that a particular amount of breast tissue be removed.
Excessively large breasts can cause pain in the upper and lower back, neck and shoulders. Well fitted bras can be difficult to find and their straps can cause shoulder grooving. The folds under and between the breasts can develop hard to treat rashes from retained moisture. Large breasts can make exercising impossible, leading to weight gain and other health problems.
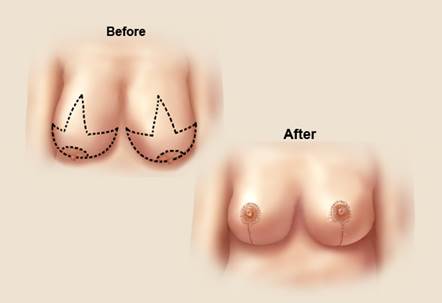
So to decrease these symptoms insurance companies cover breast reduction if a significant reduction in weight can be achieved. How much depends on your height, weight and the insurance company. For example, Blue Cross/ Blue Shield of Massachusetts requires 325 grams of tissue be removed from each breast in a woman of normal weight and height between 5’2” and 5’4”. That translates to about 2/3 of a pound, which will bring a DD cup to about a C cup.
Why suffer any longer? Come in for a consult. Breast Reduction is usually done as an outpatient with little post-operative discomfort and limited time off from work. Why don’t you take a little weight off your chest?